Retinal detachment Surgery
چهار شنبه 8 فروردین 1397
بازدید: 2213
What is retinal detachment?
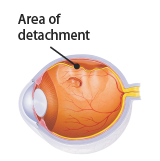
Similar to the film in a camera, the retina is responsible for "creating" the images that we see. It is the light-sensitive layer of tissue that lines the inside of the eye and sends visual messages through the optic nerve to the brain. When the retina detaches, it is lifted or pulled from its normal position. If not promptly treated, a retinal detachment can cause permanent vision loss. In cases where small or large areas of the retina are torn, these retinal tears or retinal breaks can lead to retinal detachment if left untreated.
When the retina detaches, it separates from the back wall of the eye and is no longer connected to the single layer of cells known as the retinal pigment epithelium. These cells are critical for the health of the detached retina, which will degenerate and lose its ability to function if it remains detached.
The center of the retina is called the macula, which is the only part capable of facilitating fine detailed vision. A healthy macula is necessary for reading and recognizing faces. An untreated retinal detachment continues to spread until eventually it affects the macula. If the macula becomes detached, central vision can be lost.

Here's what a person with normal vision sees

This is what that same image looks like
to a person with a retinal detachmnet
Who is at greatest risk for a retinal detachment?
A retinal detachment can occur at any age, but it is more common in people over age 40. It is also more likely to occur in those who:
- Are extremely nearsighted (myopia)
- Have suffered a retinal detachment in the other eye
- Have a family history of retinal detachments
- Have had cataract surgery
- Have other eye diseases or disorders, such as uveitis, degenerative myopia or lattice degeneration
- Have had eye trauma
What are the symptoms of a retinal detachment?
Symptoms include a sudden increase in either the number of floaters—little specks that float in and around your field of vision—and/or light flashes in the eye. Both of these conditions can be accompanied by the sensation of looking through cobwebs. Another symptom, one that tends to manifest later, is the appearance of a "dark curtain" over part or all of the field of vision.
Let us be clear on this: A retinal detachment qualifies as a medical emergency. Anyone experiencing any of the symptoms of a retinal detachment should see a retina specialist immediately.

How do floaters develop, and if I have them, does that mean that I have a retinal detachment?
Typically for people between the ages of 40 and 70, the gel (vitreous) in the center of the eye separates from the back wall of the eye, causing posterior vitreous detachment, or PVD. This is a normal part of aging and often causes floaters. PVD appears as dots, spots or curly lines that tend to move within your eye. Since the gel often pulls on the retina as it separates, this can cause flashes of light and also produce broken blood vessels in the retina, causing a vitreous hemorrhage. Small amounts of blood are often described by patients as a "shower of spots." Larger hemorrhages can create large dark blobs in the visual field or an overall decrease in vision.
If the gel remains attached to the retina, or the retina is weak in a certain area, a retinal tear can occur as the gel tries to separate from the retina. The detection and treatment of retinal tears are both described below. It is fortunate that a great majority of PVD's don't cause retinal tears. In some cases, a PVD can occur without any symptoms, and in others, the person can experience many of the symptoms without suffering a retinal break or tear.
Developing floaters does not necessarily mean you have a detached retina, but you should still see your retina specialist immediately upon the onset of the condition.
How are PVD's treated?
In most cases, PVD's do not require treatment. The floaters, although bothersome to varying degrees, usually go away after several weeks or a couple of months. For some of those people who find the floaters to be impacting their day-to-day life in a more persistent fashion, a vitrectomy is an option for achieving relief.
How are retinal tears and detachments detected?
Retinal tears and detachments are detected during a comprehensive eye exam. After having your vision and eye pressure checked, drops are placed in your eyes to widen, or dilate, the pupils.
First, your retina specialist will use a special magnifying lens to check the health of both eyes. He or she will then use a special instrument to lightly press around the outside of your eye in an effort to detect any retinal tears or detachment. An ultrasound may also be ordered if your doctor's view of the retina is not clear. Cloudiness is often caused by bleeding during the course of the PVD; this is even more suggestive of a retinal tear than a PVD without a hemorrhage. Following the exam, your close-up vision may remain blurred for several hours due to the dilating drops.
How are retinal tears treated?
Not all retinal breaks need to be treated. Many people have small holes in their retina that don't affect their vision and almost never produce associated symptoms. In general, however, if a retinal break is discovered in association with new symptoms or there is evidence of other high risk factors for a retinal detachment (previously described), one of two methods of treatment is indicated:
Laser Photocoagulation
Treatment spots are made around the tear to create a seal and keep fluid from accumulating underneath the retina.
Cryopexy
This technique freezes the area around the tear in order to seal the retinal break. This method is used when there is a large amount of blood and the laser cannot effectively reach the retina.
If retinal breaks are promptly identified, both treatments are highly successful in avoiding subsequent retinal detachment. Both of these procedures can be performed in all of The Retina Group of Washington offices.
It is unfortunate that some retinal tears progress to detachment almost immediately, sometimes without any symptoms. If this occurs, your retina specialist will recommend surgical repair.
What are the different types of retinal detachments?

Although there are three types of retinal detachments—rhegmatogenous, tractional and exudative—the first one makes up a large majority of cases. Rhegmatogenous (pronounced "reg-ma-TAH-jenous") is the type of retinal detachment that occurs when a tear or break in the retina develops. Fluid then seeps through the tear, lifting the retina from its normal position like a bubble underneath wallpaper.
Retinal tears are the most common cause of rhegmatogenous retinal detachments; these and other retinal breaks develop most often in the peripheral retina. Patients often describe a curtain or dark shadow involving the peripheral vision that enlarges as the detachment extends towards the macula (center of the retina). Central vision will be lost if the macula detaches. Without surgical repair, most rhegmatogenous detachments will eventually affect the entire retina and all vision will be lost. Chronic untreated retinal detachments may eventually lead to a blind painful eye condition known as phthisis bulbi.
How are retinal detachments treated?
Retinal detachments are most often repaired surgically by a retina specialist. Depending on the nature of your detachment, he or she will determine which specific procedure to pursue. Based on the variables, either one or a combination of the following operations is recommended:
Scleral Buckle Surgery
Scleral buckle surgery is a long established technique used to repair a retinal detachment. It is a method of closing breaks and flattening the retina. A small, invisible synthetic band, usually made of silicone rubber, is attached to the outside of the eyeball to gently push the wall of the eye against the detached retina. This relieves the traction caused by retinal breaks and also displaces some retinal fluid away from the break. Different sizes and types of scleral buckles may be used depending on the nature of the detachment.

Single operation success rates for scleral buckle, in general, are high. The operation is often performed as outpatient surgery and does not typically require an overnight hospital stay.
Following the procedure, your retina specialist may recommend you remain in a particular position during recovery in order to increase the chance of a successful result. You may experience some pain for a few days after the surgery; your eye may be swollen, red and/or tender for several weeks. You may be asked to put drops in your eye to help prevent infection and to keep the pupil from constricting. It may also be necessary to wear a patch over the eye at night.
A common side effect of scleral buckle surgery is increased nearsightedness. There are many less common complications that include eye infection, increased eye pressure, bleeding, injury to other parts of the eye, cataract, droopy eyelid and double vision. Complete vision loss is very rare, but possible as a result of scleral buckle surgery. As this procedure can change the shape of the eye, your prescription will likely change and you will ultimately need to have your contact lens or glasses prescription checked. If the initial operation is unsuccessful, additional surgery is likely to be recommended.
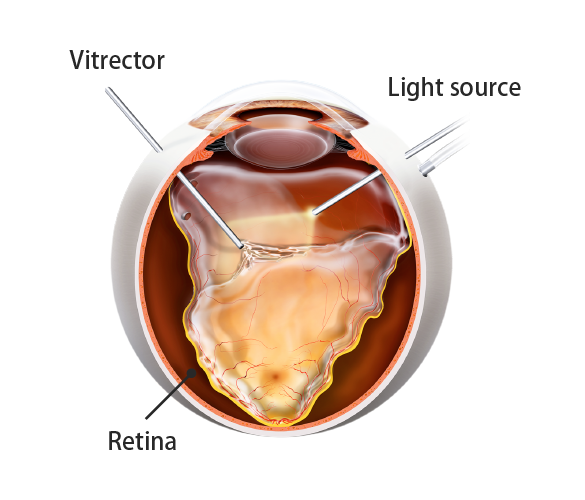
Pars Plana Vitrectomy
During a vitrectomy, the doctor makes three small incisions in the sclera (white of the eye). The vitreous, a gel-like substance that fills the eye, is removed using a small instrument. The fluid under the retina is then drained and laser treatment is applied to the tear and any other weak areas of the retina. Gas or silicone oil is then injected into the eye to replace the vitreous, reattach the retina and keep fluid from getting through the retinal break and detaching the retina again. Your doctor may ask you to position yourself face down or on your side in order to allow the gas or silicone oil to work most effectively to prevent fluid from getting under the retina during the early post-operative period.
Gas
During the healing process, the eye makes fluid that gradually replaces the gas. Because the gas is reabsorbed spontaneously, surgery to remove the gas is not needed. Different types of gas bubbles are used which can last in your eye for up to two months. Certain travel restrictions may apply while gas is present.
Silicone Oil
This may be used in the place of gas for more complex or recurrent detachments. Silicone oil does not reabsorb spontaneously and needs to be removed by a second surgery.
Regardless of whether gas or silicone oil is used, the single-operation success rate for vitrectomy is high. It is often performed on an outpatient basis and does not typically require an overnight hospital stay.
Complications are similar to those from scleral buckle surgery, even though the procedure doesn't always create more nearsightedness. It does, however, result more predictably in cataract formation. If this procedure is unsuccessful, your retinal specialist will likely recommend additional surgery.
Pneumatic Retinopexy
During a pneumatic retinopexy, a gas bubble is injected into the center of the eye to temporarily prevent fluid from entering through the retinal tear. Laser or cryopexy is then used to create a permanent seal. The specialized retinal pigment epithelial cells are then able to pump the existing fluid out from behind the retina. This procedure relies on the patient's ability to position their head so the small gas bubble stays over the retinal tear. For this reason, pneumatic retinopexy may not be the appropriate procedure for all retinal detachments. In select circumstances, the success rate of this procedure is high.
Pneumatic retinopexy is typically done in your retina specialist's office and can be performed at all of The Retina Group of Washington locations. As with other surgical procedures to repair retinal detachments, this has potential complications that include new post-operative retinal breaks, increased eye pressure, infection, gas getting behind the retina and cataract formation. Total visual loss is rare, but possible following this operation. Here again if this procedure is unsuccessful, your doctor will likely recommend additional surgery.
Medical Health
Depending on your overall health, your retina specialist may ask you to see your primary care provider for a general health check prior to retina surgery. Be sure to let your surgeon know if you have any serious medical conditions or allergies and if you are on blood thinners or other medications that slow clotting of your blood.
Recovery
You should arrange to have someone drive you to your follow-up doctor's appointment after surgery. The doctor may advise you to maintain a certain position for several days after surgery. Ask if you need to restrict activities at home and/or at work for a period of time. You will need to use eye drops several times a day for several weeks.
How soon will my vision return after surgery?
The answer depends on several factors, including which procedure was performed and how much of the retina was detached prior to the surgery. A gas-filled eye will have limited vision for several weeks until the gas bubble is naturally reabsorbed. Silicone oil allows more clarity than gas, but will still cause blurry vision until your doctor removes it.
What should I expect in the long run?
With the use of modern therapy, over 95% of those with a retinal detachment can be successfully treated, even though multiple operations may be needed. Many patients retain excellent vision, but the outcome is not always predictable. The final result may not be known for several months after surgery—and even under the best of circumstances and after multiple procedures—vision may eventually be lost. The best results come when the retinal detachment is repaired before the macula detaches. That is why you must contact a retinal specialist immediately if you see a sudden or gradual increase in the number of floaters and/or light flashes, or a dark curtain over the field of vision.
Will I need new glasses or contacts?
After you receive treatment for your retinal tear or detachment, your retina specialist may recommend that you obtain new glasses or contact lenses. It is important that you continue to have regular eye exams and inform your doctor if you have any vision changes.
REFRENCE: www.rgw.com
دیدگاه های ارسال شده توسط شما، پس از تایید مدیر سایت در وب سایت منتشر خواهد شد.
پیام هایی که حاوی تهمت یا افترا باشد منتشر نخواهد شد.
پیام هایی که به غیر از زبان فارسی یا غیر مرتبط با خبر باشد منتشر نخواهد شد.