What is Keratoconus?
The word Keratoconus, which is a Greek word, is composed of two words: Keratos, meaning cornea, and Konos, meaning cone. Keratoconus (KC) is a disease of the cornea; the cornea is the transparent, anterior layer of the eye that plays an important role in providing the eye's refractive power or the eye's ability to focus on objects and provide accurate vision.
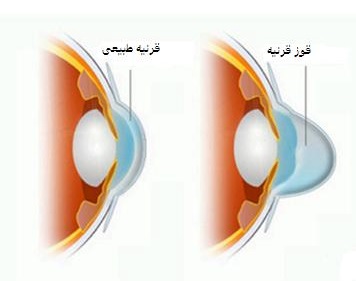
The normal cornea is regular and spherical in shape. However, when the eye is affected by keratoconus, the shape of the cornea gradually changes as the cornea bulges out, thins, and forms a cone. Due to the deformation, this condition is called keratoconus. The deformation of the cornea that occurs due to keratoconus leads to progressive vision deviation, which is usually accompanied by increasing myopia (nearsightedness) and irregular astigmatism. Figure 1 shows a normal cornea and a cornea affected by keratoconus.
Image 1 - Normal cornea and cornea with keratoconus
What causes keratoconus?
Although keratoconus has been known and studied for more than 200 years, its main cause remains unknown. Researchers around the world are trying to discover the main causes of this disease by continuing their studies on keratoconus.
There are several theories about the causes of keratoconus. According to one of these theories, the thinning of the cornea is due to enzyme damage that leads to the destruction of corneal tissue. Proponents of another hypothesis believe that some hormones, whose activity usually begins at puberty, can cause keratoconus in people. Some studies have also suggested a genetic effect on the development of keratoconus. These studies show that 15 percent of those with keratoconus have another family member with the same disease. Although keratoconus runs in families, there is a 10% chance that a person with keratoconus will pass it on to their children.
Who gets keratoconus?
The exact prevalence of keratoconus is unknown. Although it is not one of the most common eye diseases, it is not rare either. It is estimated that 2 out of 1,000 people in the general population are affected. Recent advances in advanced eye testing equipment, such as corneal topography, have made it possible to detect keratoconus in its early stages.
Keratoconus most often affects adolescents and young adults. However, it has been reported in people in their 40s and 50s. People of all races, both sexes, and from all walks of life can develop keratoconus. Figure 2 shows a topographic map of the eye of a person with keratoconus.
Figure 2 - Topography of the eye of a person with keratoconus
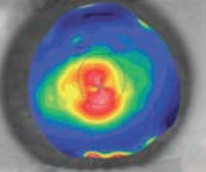
In the corneal topography, the central red area shows that the central curvature of the cornea is abnormally steep due to keratoconus.
What are the symptoms and complications of keratoconus?
The first sign of keratoconus is blurred vision, which occurs due to changes in the shape of the cornea following myopia or astigmatism caused by keratoconus. In the early stages of keratoconus, vision is usually well corrected with glasses. As keratoconus progresses and the refractive problem increases, it may be necessary to change the number of glasses regularly.
After the initial stages of keratoconus, glasses cannot provide the person with adequate quality of vision; therefore, special contact lenses may be needed. Keratoconus usually progresses over a period of 10 to 15 years and then becomes almost stable. In some cases, the progression of keratoconus may be very rapid and uncontrollable, and in advanced stages of the disease, the person may not be able to tolerate contact lenses. In very advanced cases, scarring may form on the surface of the cornea, which causes further damage to the person’s vision and may lead to vision loss. Figure 3 shows the experience of a person with keratoconus in viewing images (as blurry and distorted).
Figure 3 - Clarity of viewing images by a healthy eye (right) and an eye with keratoconus (left)

How is keratoconus treated?
Depending on the stage of progression of the disease, there are various treatment options, which we will discuss in order below.
Glasses:
In the early stages of keratoconus, myopia (nearsightedness) and astigmatism are well corrected with glasses.
Contact lenses:
As keratoconus progresses, the shape of the cornea can become very irregular, and glasses can no longer provide adequate vision. At this stage of the disease, special contact lenses are prescribed and recommended by an ophthalmologist.

There are several types of contact lenses for keratoconus. One of the most common contact lenses used is rigid gas-permeable contact lenses (RGP). In general, these contact lenses can correct myopia (nearsightedness) and astigmatism well. These lenses allow oxygen to pass through the cornea, which is necessary for breathing. RGP contact lenses used for keratoconus are custom-made for each patient.
Corneal Transplantation:
Approximately 25 percent of patients with keratoconus reach advanced stages of the disease and require a corneal transplant. Corneal transplant surgery for keratoconus patients has a high success rate. However, this treatment is a very invasive procedure.
It is considered a surgical procedure and can potentially have complications, including the risk of graft rejection.
The recovery process after corneal transplant surgery takes about a year or more. During this time, the patient will need to visit an ophthalmologist several times. Most patients still need to wear glasses or contact lenses after a corneal transplant.
(Keraring) Intracorneal Ring Segments
The implantation of intracorneal ring segments is the most advanced treatment option available for keratoconus and is used in very advanced cases of keratoconus or in patients who are no longer able to wear contact lenses due to the shape of their cornea. This implant consists of one or two semicircular pieces made of a body-compatible material called PMMA.
The use of PMMA in intraocular implants has a long history of safety and effectiveness and has been used for more than 50 years in the manufacture of intraocular lenses used in cataract surgery.
Objectives of keratoplasty
The goal of keratoplasty is to provide the patient with the following conditions:
Flatten the cornea and reduce the prominence of its conical shape.
Regularize the corneal surface, reduce visual deviations and improve the patient's quality of vision.
Reduce myopia (nearsightedness) and astigmatism caused by keratoconus. However, there is no guarantee that the patient will not need to use glasses or contact lenses after this procedure.
Slow the progression of keratoconus and stabilize the shape of the cornea. This generally eliminates or delays the need for a corneal transplant.
Increase the eye's tolerance to accept contact lenses and feel comfortable with lenses.
Kerating surgery has been used to treat keratoconus since 1995. So far, more than 100,000 patients with keratoconus in 45 countries have successfully undergone Kerating surgery and intracorneal ring implantation. According to various clinical trials and research and results published in reputable medical journals, Kerating (intracorneal ring implantation) is a safe and effective surgery for many patients with keratoconus.
The most common questions about Kerating surgery:
Based on what criteria can Kerating surgery be suitable for an individual?
In order to determine whether Kerating surgery is a suitable option for an individual, it is necessary to undergo a complete eye examination and advanced eye tests requested by the ophthalmologist. Then, the results of the tests are fully evaluated by the ophthalmologist. It is the ophthalmologist's expert opinion that, after evaluating the patient's condition, determines whether Kerating surgery can be a suitable option for him or her. In general, it can be said that Kerating surgery can be a treatment option for patients with progressive keratoconus, or those whose eyes cannot tolerate contact lenses and need a corneal transplant. In addition to these patients, other people who can benefit from Kerating surgery include: patients in whom keratoconus has developed following laser vision correction; patients with severe corneal irregularities that have developed following radial keratotomy surgery; and patients with severe irregular astigmatism that has developed following corneal transplantation.
Who is Kerating surgery contraindicated for?
Patients with severe keratoconus or those with large scars on the cornea are not suitable for Kerating surgery; patients with allergies who have a habit of rubbing their eyes may experience severe complications after the procedure if they undergo this type of surgery. Therefore, their allergic disease should be treated before the operation to avoid rubbing the eyes after the operation. Patients who expect not to need to wear glasses or contact lenses after the operation should consult their doctor about the possible benefits of this operation before undergoing this operation; because the surgery of the cornea is not a refractive surgery that completely eliminates the need for glasses or contact lenses.
How long do the results of the surgery of the cornea remain effective?
The results of the surgery of the cornea for the patient have no time limit and do not change until the end of life. There are patients who underwent this operation in 1995 (the first year of the use of this medical technique) and the result of the operation is stable and successful for them. The intracorneal ring is made of a polymer compatible with the human body called PMMA. This material has been used to make intraocular lenses since 1949 and so far there have been no reports of graft rejection or deterioration of quality over time. Although the quality of the results of the procedure has not changed in most patients over the years, it is possible for keratoconus to progress and in some cases a corneal transplant may be required.
Is the ring implanted in the cornea visible to others?
The ring used in keratoconus surgery is clear and very small. In terms of appearance and cosmetic effect, it is similar to contact lenses and in most cases is not visible to the naked eye by other people.
What should the patient do before going for keratoconus surgery?
If you wear contact lenses, according to your doctor's instructions, you should not wear them for several days before the procedure to allow your eyes to return to their normal condition. Before going to the center for the procedure, eat a light meal, take a shower, and wash your hair.
Do not use any makeup, especially around the eyes. Do not use any perfume or fragrances. Be at the hospital at the appointed time on the day of the operation. Before entering the operating room, the nurse will put some special eye drops in the eyes to prepare the eyes for surgery. Then, you will be asked to change your clothes and put on a special operating room gown to prepare for the sterile operating room.
How is the cryotherapy surgery performed?
Cryotherapy surgery is a quick and painless procedure that is performed on an outpatient basis without hospitalization. Anesthetic eye drops are instilled into the patient's eye to numb the eye. The patient is conscious during the operation but does not feel any pain. The surgery is performed in the operating room under completely sterile conditions. The surgeon uses a high-precision surgical microscope to have a very clear and precise view of the inside of the eye.
Cryotherapy surgery is performed with the help of special microscopic equipment designed for this surgery. By making a 1 mm incision and a tunnel in the thickness of the cornea, the desired ring is implanted into the cornea. In most cases, the incision site heals on its own and no stitches are needed. After the operation, the patient is transferred to the recovery room to rest for a short time and reach a stable condition before being discharged from the hospital. After examination and checking the symptoms, the patient is discharged and can go home.
What should the patient do during the postoperative recovery period?
Corneal ring surgery is a less invasive surgery. Therefore, the patient can resume most of his daily activities 2 to 3 days after the operation.
It is expected that you will have symptoms such as blurred vision, redness of the eyes, itching, burning, sensitivity to light and fear of light for a few days after the operation. These symptoms are completely normal after the operation and will improve with the use of medications and eye drops that the doctor has prescribed for use after the operation. It is very important to take all medications as prescribed by your doctor and at the right time and to follow your surgeon's recommendations carefully. If these symptoms are absent and begin a few days after surgery, it is abnormal and you should discuss this with your doctor immediately.
In many patients, vision improvement is noticeable a few days after surgery, however, stabilization of the person's vision takes an average of approximately 12 weeks. During this time and before final stabilization, it is completely normal for the person's vision to vary and fluctuate. Since intracorneal ring implantation and kerating surgery are not designed to correct refractive errors of the eye, the person may need to wear glasses or contact lenses after surgery. In such cases, the doctor will prescribe temporary corrective glasses after a month and after the person's vision stabilizes (approximately 3 months after surgery), permanent glasses with a final and stable number are prescribed.
What are the risks of kerating surgery?
As with any surgical procedure, there are risks involved. For example, in cases where the corneal tunnel is very difficult to create, the surgeon may decide to forgo the ring implant during the procedure. There is a very small chance of infection after the procedure, especially if you do not take your prescribed medications regularly and as prescribed or if you are exposed to environmental contamination. If an infection occurs, the surgeon may decide to remove the ring implanted in the cornea from the eye. Other possible complications after corneal ringing surgery include protrusion or displacement of the implanted ring. If these occur, the ring is surgically fixed in place or, at the surgeon's discretion, removed altogether. At any time after the procedure, the surgeon may decide to change or reinsert the intracorneal ring to improve the outcome. If the intracorneal ring is removed, the cornea returns to its previous shape and condition before the procedure. Therefore, the patient's condition will also return to its preoperative condition. The probability of mild complications after the procedure is approximately 3%. The incidence of serious complications is less than two-tenths of a percent. It is worth noting that in the event of serious complications, this is an emergency situation and may require an emergency corneal transplant.
What can be done during the postoperative recovery period to reduce the risk of complications?
You should take all medications and eye drops prescribed by your doctor regularly and at specific times. Given that you should stay away from any environmental pollution, you should avoid swimming, going to the sauna, doing heavy exercise, and rubbing your eyes for at least a month after the operation. When showering, be careful not to get water in your eyes. The eyelids should always be kept clean. To do this, you should clean the eyelids with saline solution and sterile gauze obtained from the pharmacy. When you intend to use eye drops, wash your hands with soap and water before touching them. Be careful not to let the dropper tip come into contact with your hands or eyes. Close the container lid immediately after use.
Avoid being in polluted environments or places where many people are present or frequent for at least a month after the operation. Your doctor may advise you to cover your eyes with an eye protection patch before going to bed. This will prevent you from touching your eyes and rubbing them unconsciously while you sleep.
It is essential to keep your post-operative visits on the dates given to you. Typically, visits are made one day after the operation, one week after the operation, and then 3, 6, and 12 months after the operation.
What is the success rate of this procedure?
The success rate of Keraring surgery depends on the severity and progression of the keratoconus. Patients with mild to moderate keratoconus will experience better results than those with advanced keratoconus. According to statistics, the success rate of Keraring surgery in mild to moderate keratoconus is 96%.
What are the advantages of keratoconus surgery compared to corneal transplantation?
Faster vision recovery (3 months compared to a year for corneal transplantation)
No risk of rejection
Easier contact lens wear after surgery
Reversible if needed
Delays the need for corneal transplantation or eliminates the need for it altogether
Is corneal transplantation better than keratoconus surgery?
The success rate of corneal transplantation for patients with keratoconus is over 90%. However, corneal transplantation is a very invasive surgery and has a long recovery period (a year or more). There is also a possibility of graft rejection at any time. If graft rejection does not respond to conventional treatments, a corneal transplant may be required. It should be noted that the success rate of the procedure is greatly reduced in corneal transplants.
After a corneal transplant, in most cases, the patient will need to wear glasses and contact lenses. Corneal transplantation is completely dependent on the availability of a corneal donor, so the patient may have to wait a significant amount of time to receive a donated cornea from an eye bank.
Can corneal transplantation be avoided by performing keratoconus surgery?
The main goal of keratoconus surgery is to restore the quality of vision in patients with keratoconus. Many patients who have undergone keratoconus surgery and their corneal shape has stabilized confirm that this procedure can delay their need for a corneal transplant indefinitely or completely eliminate it.
Intracorneal Ring (Kerating Surgery)
You can consult your ophthalmologist for more information about keratoconus (corneal curvature) and its treatment options.